What is a Kyphoplasty?
Balloon Kyphoplasty is a minimally invasive procedure for the treatment of vertebral compression fractures, commonly called spinal fractures. This type of fracture is often caused by conditions that affect bone mass such as osteoporosis, cancer, or long-term use of oral corticosteroids. Spinal fractures cause the vertebral body to crack or collapse, altering the shape of the spinal column. Just one fracture can change the vertical alignment of the spine and can lead to additional fractures.
It has been estimated that over 700,000 spinal fractures occur annually in the U.S. alone. Significant pain and some degree of kyphosis is common, especially in patients suffering from multiple fractures.
Before minimally invasive surgery, the only treatment option for patients with spinal fractures was open surgery. Outcomes were poor, primarily because attaching hardware to bone that is already “soft” or compromised is difficult and not successful. Balloon Kyphoplasty is an innovative technique that can restore the vertebra to a near-normal shape, thereby maintaining spinal alignment. Before the procedure, the patient usually undergoes imaging studies to pinpoint the location of the fracture. Many patients report immediate relief from pain after the procedure due to the exothermic reaction of the bone cement hardening process.
What is a lumbar epidural steroid injection?
During this procedure, a corticosteroid (anti-inflammatory medicine) is injected into the epidural space to reduce inflammation and pain. Your physician may inject into the epidural space from behind, this is called an interlaminar injection. When your physician goes in from the side, it is called a transforaminal injection. If the needle is positioned next to an individual nerve root, it is called a selective nerve root block. When performed from below it is called a caudal injection.
What does a Kyphoplasty procedure entail?
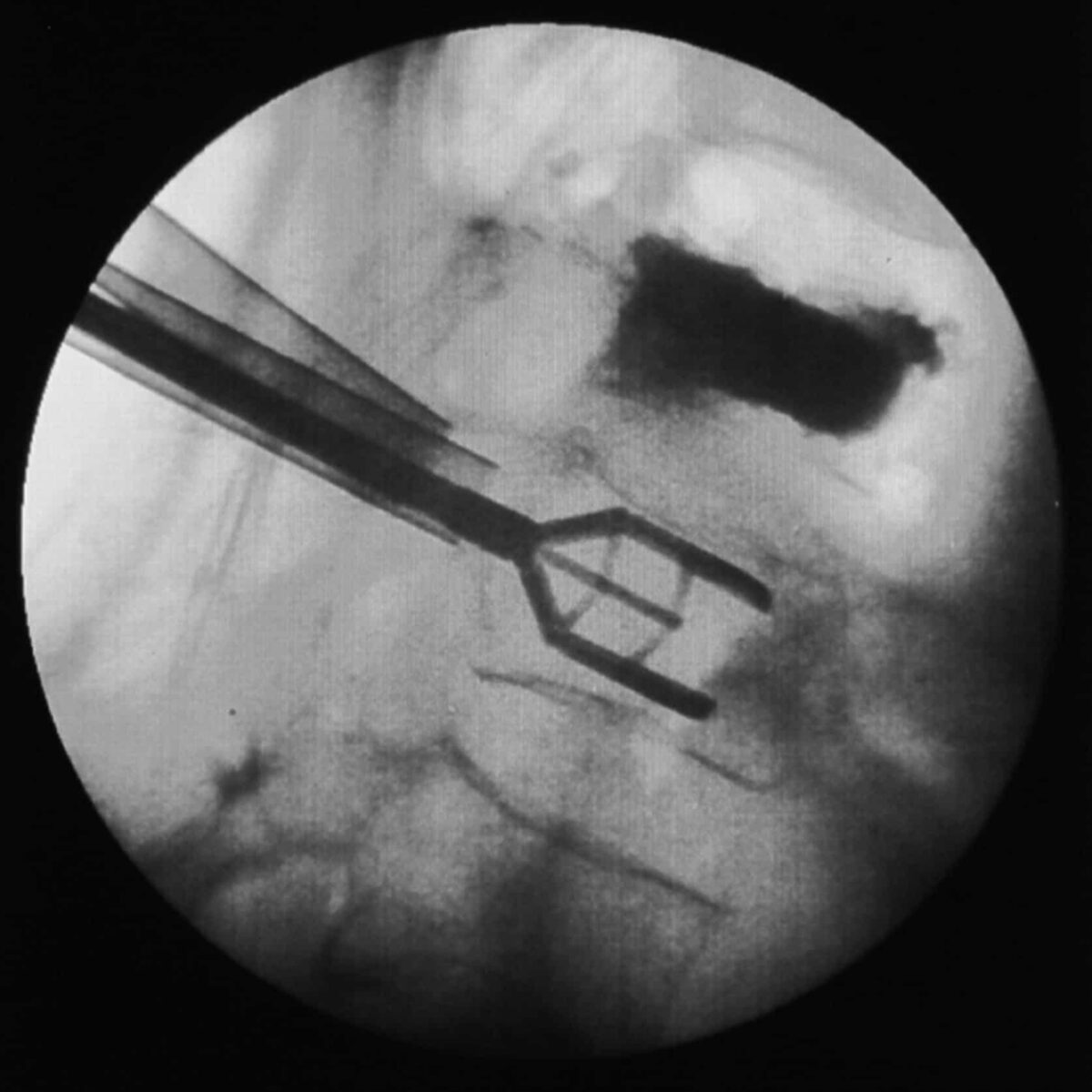
Through two small incisions on either side of the spine, the spine specialist inserts a trocar into the fractured vertebra under fluoroscopic guidance. One to two small orthopedic balloons are passed through the trocar and inflated inside the collapsed vertebral body. Inflation of the balloons raises the collapsed vertebral body in an attempt to restore normal anatomy.
Once height and shape of the vertebra has been restored, the balloons are deflated and removed. The “hollow” or void created by the balloons are then filled with bone cement. The bone cement hardens quickly, creating an internal cast thus stabilizing the fracture.
Do I need to be in the hospital for a Kyphoplasty?
Balloon Kyphoplasty may require an overnight hospital stay, depending on medical necessity. This procedure is typically performed on an outpatient basis. The procedure takes about one hour per fracture level treated and many patients are able to resume normal activity rather quickly.