What is Sacroiliac Joint Pain?
Sacroiliac joint pain or SI joint dysfunction is the result of too much or too little motion occurring at the sacroiliac joint, which leads to inflammation and pain, which can often be debilitating. Part of the pelvis, the SI joint is attached to the front and back by the muscles and ligaments which surround it. Any of these can be the source of pain in a dysfunctional SI joint.
What are some symptoms of Sacroiliac Joint Pain?
Pain can range from dull aching to sharp and stabbing and increases with physical activity. Symptoms also worsen with prolonged or sustained positions (i.e., sitting, standing, lying). Bending forward, stair climbing, hill climbing, and rising from a seated position can also provoke pain. Pain is reported to increase during menstruation in women and sexual intercourse. Some examples include:
- Lower back & buttock pain
- Sciatic leg pain
- Groin pain & hip pain
- Knee Pain
- Transient numbness
- Urinary frequency (rare)
How is Sacroiliac Joint Pain Diagnosed?
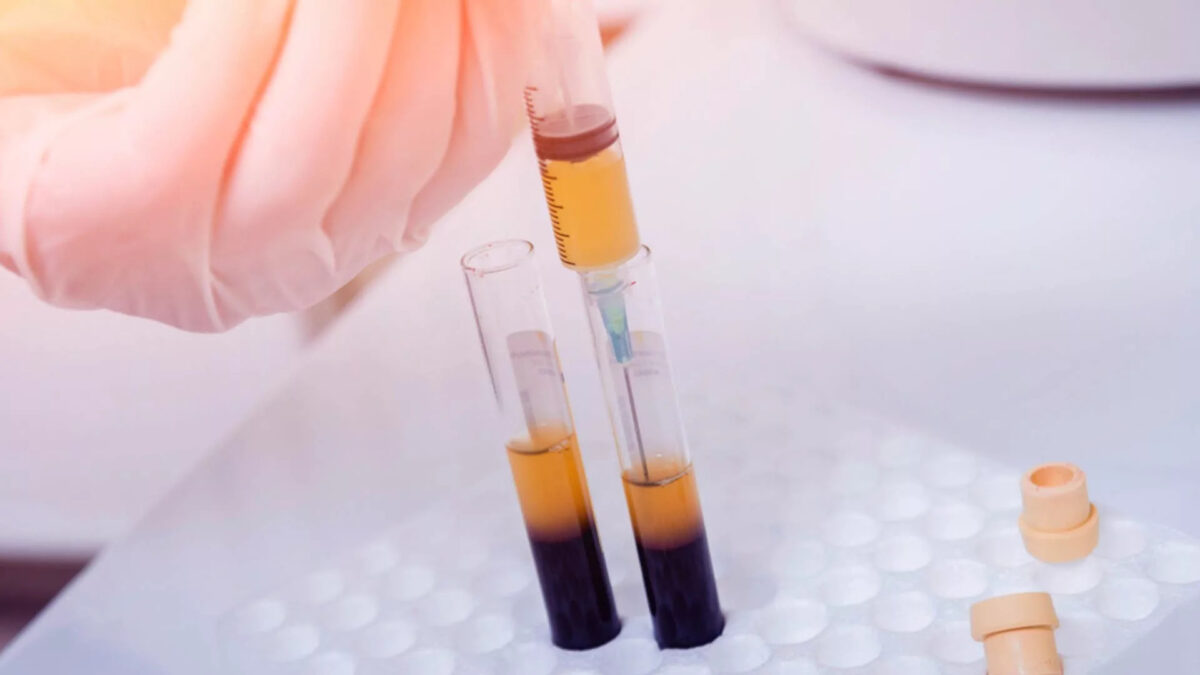
Certain physical exam findings correlate with SI joint pain and dysfunction. The current “gold standard” for diagnosis of sacroiliac joint dysfunction emanating within the joint is a sacroiliac joint injection confirmed under fluoroscopy or CT-guidance using a local anesthetic solution.
How do you treat Sacroiliac Joint Pain?
Treatment is often dependent on the duration and severity of the pain and dysfunction. In the acute phase (first one to two weeks) for a mild sprain of the sacroiliac, it is typical for the patient to be prescribed rest, ice/heat, physical therapy, and anti-inflammatory medicine. If the pain does not resolve in the first one to two weeks, then the patient may benefit from a steroid and anesthetic mixture injected via into the joint with fluoroscopic guidance (this also serves in confirming diagnosis).
For the most severe and chronic forms of sacroiliac dysfunction, treatment should proceed with the support of a sacroiliac belt, and a series of prolotherapy injections to aid in regeneration and healing of the surrounding injured ligaments. If that treatment is limited, surgical transection of the sacral lateral branch nerves may be appropriate if pain relief is confirmed with a series of lateral branch blocks confirmed under fluoroscopy.